Over the last 10 years, Orthopedic Surgeons have embraced the
concept of lowering the cost of joint replacement surgery in the U.S. In
addition to cost reduction, we have taken steps improved outcomes,
increasing value by delivering better care at lower prices.
Primarily, we have lowered
costs by shortening the length of stay after joint replacement. Thirty years ago, the typical length of stay
was seven days, a huge contrast to our current day paradigm allowing 80% of our patients go
home the same day.
Additionally, by focusing attention on pre-op optimization (weight loss, smoking
cessation, diabetes management, among others), we have decreased ER visits and
re-admissions to the hospital dramatically. We have also dramatically reduced
the use of post-discharge care facilities (which was further hastened by COVID-19).
All of these changes required more work from the orthopedic surgeons and their
care teams.
In a recent article in the July 2022 issue of Journal of Arthroplasty, Bernstein et al. outline how this work by orthopedic surgeons has reduced the cost of care to Medicare but the reimbursement to orthopedic surgeons has consistently decreased despite the significant savings.
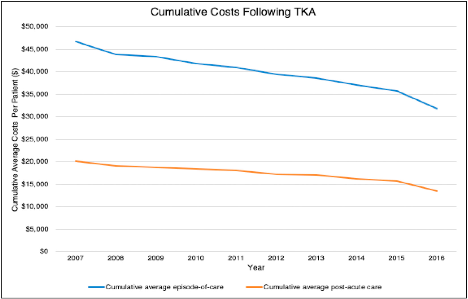
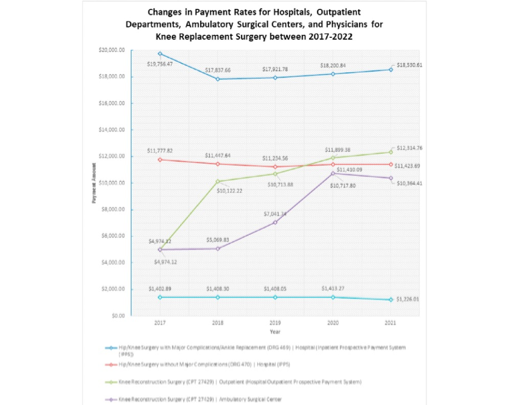
This chart shows a reduction in overall costs from 2007 to 2016 of $15,000. That is the cost not what Medicare pays hospitals which is substantially less. See chart below which tracks the reimbursement to hospitals and surgery centers over time. As you can see the reimbursement to hospitals has remained relatively stable while the reimbursement for surgery centers has increased but remains well below what hospitals receive.
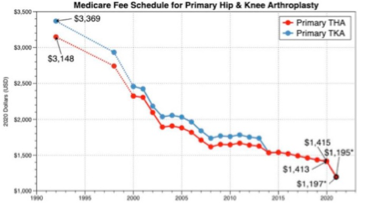
The chart above shows the reimbursement to surgeons over the
last 30 years which has steadily declined from S3,200 to $1,200 per procedure
and this fee covers surgeon services for the procedure and 90 days of
follow-up. All the while the cost of living and overhead have increased.
So, while orthopedic surgeons have played a pivotal role in
lowering costs and improving quality we have been subjected to dramatically
reduced reimbursement. This makes access to care more challenging for Medicare
patients as surgeons limit the number of Medicare patients they see.
Conclusions
While surgeons have worked with insurance companies and
Medicare to lower costs and improve quality for joint replacement surgery, they
have seen progressive erosion of reimbursement for hip and knee replacement
surgery. While Medicare patients are some of the most appreciative patients,
challenges confront orthopedic practices and hospitals regarding how to
maintain high quality care in the face of continually decreasing reimbursement.

