I have had the privilege of writing a chapter on results of Direct Anterior Approach (DAA) for total hip replacement (THR). This chapter is for an upcoming book on Anterior Hip replacement.
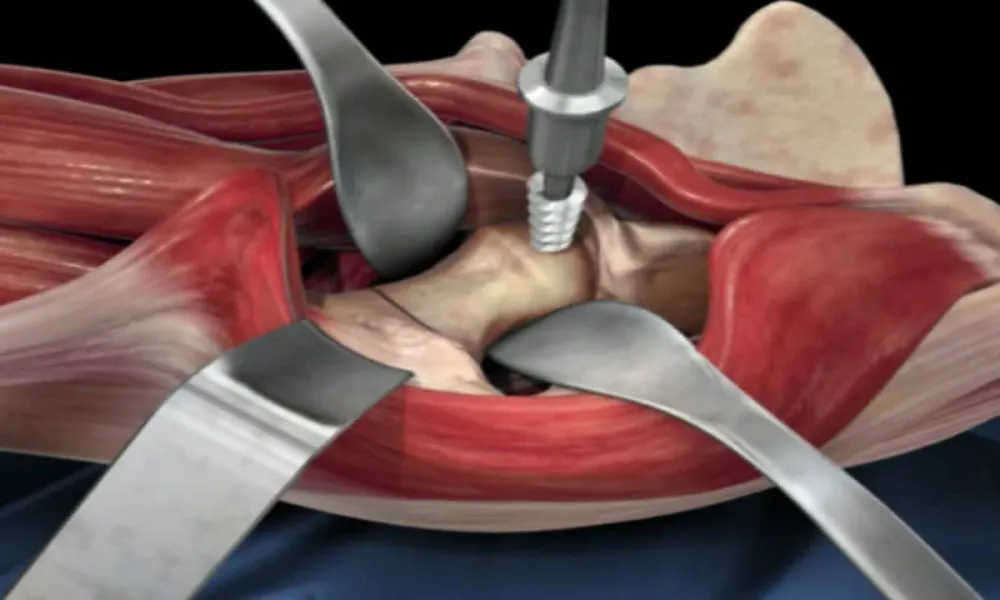
The DAA for THR uses a true intermuscular / internervous interval to approach the hip. It stands to reason that this approach if properly done should result in less soft tissue / muscle damage. The early results (2003-2005) using this approach gave reassurance it could be safely performed with a reasonable rate of complications in the hands of experienced surgeons. With interest in less invasive / minimally invasive approaches to the hip increasing approximately 15 years ago, surgeons began to explore / adopt the DAA. Studies reported after the early results included surgeon's learning curve experience. It became clear that surgeon experience, preparation and mentoring impacted outcomes with DAA. The drawbacks of limited preparation and low surgical volume prior to adopting the DAA were revealed in the study by Woolson and others. The value of diligent preparation, learning and planning was demonstrated in studies by other authors.
I started performing DAA THR in 2008 after extensive training and visiting surgeons who had been performing this procedure. Results from more recent studies reveal some trends. DAA THR is associated with less pain, earlier functional recovery, more accurate implant placement, which translates into a lower dislocation rate. Most of these advantages occur in the first 3 months postoperatively. The theoretical advantages of this approach have been documented by MRI and inflammatory markers.
Has marketing and hype contributed to the popularity of this approach? One could argue it has played a role. However, as use has become more widespread and residents and fellows are learning the DAA as part of their training its growth is more organic versus resulting from external forces. There is a saying in Orthopedic circles that Orthopedic surgeons use data much like a drunk uses a lamp post: more for support than illumination. In the 2 papers I have published in the Journal of Arthroplasty in 2013 and 2019, my experience with DAA has confirmed that my patients get better faster and have lower complications when compared to patients who had a posterior approach for THR.
So what do I tell my patients regarding why I use the DAA for all my cases?
"It is associated with less pain, a faster recovery and return to activity which in my experience lasts for approximately 3 months. Due to use of intraoperative fluoroscopy and a software program I am more accurate with my implant placement and this allows me to better address limb length and hip biomechanics. This results in a short and long term reduction in the risk of dislocation".